Contrast induced Acute Kidney Injury (CI-AKI), is commonly defined as either an increase of serum creatinine (SCr) of more than 0.5 mg/dL or more than 25% from baseline after 48 hours post-exposure to contrast media (Ozkok 2017). CI-AKI remains to be a dreaded complication following procedures usually requiring iodinated contrast. Controversy still exists in its diagnosis and management with monitoring and prophylactic protocols differing both internationally and locally.
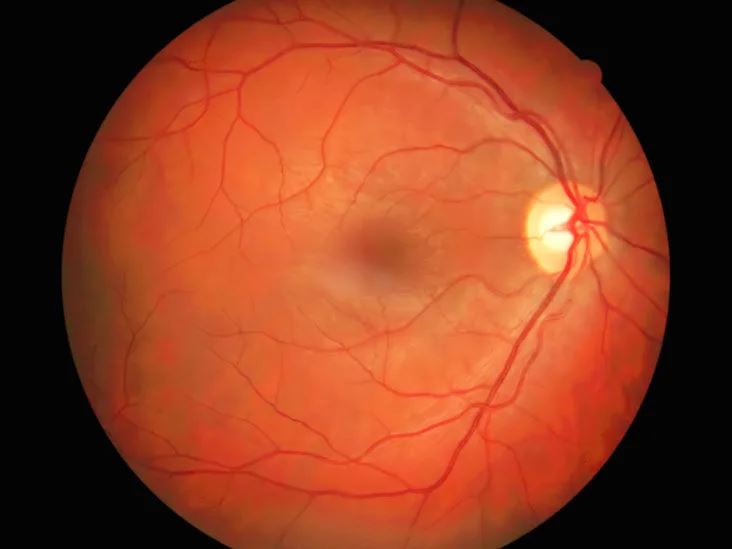
Fluorescein Angiography (FA) is a common diagnostic tool which uses a sodium fluorescein, a non-iodinated contrast, to visualize the retina. The widespread use of this modality in patients with both diabetes (DM) and chronic kidney disease (CKD) has led to a debate as to whether this type of contrast procedure may affect kidney function significantly or whether keen monitoring of kidney function and nephrology consultation is warranted prior to its conduct.
To date, there are no established standard or local protocols with practices varying depending on institutional requirements. Most centers necessitate repeat laboratory tests and nephrology subspecialty clearance in patients with elevated SCr, cut-off values of which still differ per center. Medical clearance along with routine testing of laboratories has led to some delays in imaging and management as well as unwarranted costs for patients. Hence, there is a need to review recent data and establish a consensus regarding the association of FA and CI-AKI, specifically in patients who are more prone to acute kidney injury (AKI) such as those with CKD.